The board-certified physicians at the Gastro Care Institute have significant experience in treating conditions, diseases and disorders that affect our patients’ digestive and gastro wellness. This expertise, and our practice’s continued focus on utilizing the latest techniques and advanced technology during treatment, have helped us establish a reputation as a leader in gastro health care in Southern California. We are dedicated to providing a high-level of gastro care that is personalized, collaborative and patient-focused.
Colonoscopy
People age 50 and older should have a colonoscopy, a procedure that identifies and diagnoses conditions that affect your colon.
During a test that typically takes around half an hour, your doctor will administer anesthesia After this your entire colon is scoped, providing a full view of the large intestine. Any suspicious area will be tested through a small sample that is removed, and you may be moved to your back if needed to assist the colonoscopy. This is a critical tool that can be used to identify, diagnose, and eliminate abnormal, differently-sized growths (from a dot to several inches in size) that may be located in your intestine’s wall and can be harmful to your health
How to Prepare for your colonoscopy.
Downloadable Forms
Colonoscopy Information Form
2-Day Colonoscopy Prep Form
Golytely Instructions Form
Miralax Instructions Form
MoviePrep Instructions Form
Nulytely Instructions Form
Clenpiq Instructions Form
Suprep Instructions Form
Capsule Endoscopy
Offering a video of a person’s small bowel that otherwise cannot easily be captured through a traditional endoscope or a colonoscope, a capsule endoscopy uses a small camera to view your GI tract. This camera sends images (at a rate of two frames per second) to a portable computer affixed to a belt worn by the person undergoing the capsule endoscopy. This camera is delivered through a pill that travels through your body’s digestive system over the course of eight hours.
- MiroCam
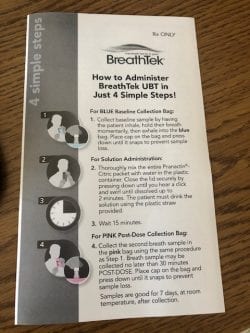
- Breath Tek
- CRH Medical Corp.
Capsule endoscopy is performed to address the following issues:
- Chronic abdominal pain
- Persistent diarrhea
- Unusual images of your GI tract
- Polyposis syndrome (a genetic form of colon and rectum cancer)
- GI blood loss
- Crohn’s disease
How You Can Prepare
Downloadable Forms
Pre Capsule Endoscopy Forms
Capsule Endoscopy Forms
Post Capsule Forms
Endoscopic Ultrasonography (EUS)
To detect potential Barrett’s esophagus, pancreas conditions, lymphoma, and lung, stomach, rectal, colon, or other cancers, doctors often use an endoscopic ultrasonography (EUS) procedure. An EUS studies your gastrointestinal (GI) tract the identify and diagnose GI tract conditions.
Prior to the start of your EUS, you will be sedated and your throat anesthetized for a review of your upper GI tract. When examining the lower GI tract, the level of sedation you receive depends on the length of, and the area of the colon to be reviewed by, the EUS procedure.
EUS is vital to detecting many serious and life-threatening medical conditions, including lumps and lesions that may be cancerous and can affect your body’s digestive and respiratory system and other areas. It can also reveal the presence of lymphoma, bile duct stones, Barrett’s esophagus, sarcoidosis, pancreatitis and pancreatic cysts, conditions that cause abdominal pain/weight loss, and other matters.
Downloadable Forms
ERCP Form
Hepatitis Management
A higher level of liver enzymes is generally a sign of Hepatitis C Virus (HCV). However, there are typically no other signs of HCV. Once hepatitis C is confirmed, additional tests will also be ordered, including a confirmation of the presence and active nature of the infection as well as the type of hepatitis C you are infected with.
For those with liver damage, being obese will increase your chances of contracting cirrhosis due to an increase in HCV-related inflammation (through increased scarring of the liver). Staying within 10 percent of your ideal weight is critical to battling liver damage. Alcohol is a primary factor in driving the progress of hepatitis C and the spread of liver failure, and will also combat anti-HCV drugs. Your physician will most likely recommend that that you stop drinking alcohol.
Remicade Infusion
Remicade® (infliximab) is the newest medication used to treat Crohn’s disease and ulcerative colitis. It is given by a medical professional via an IV infusion over a two-hour period and is used to suppress inflammation in the gut. Some patients may need to take another medication prior to the infusion to prevent or reduce possible side effects of the drug.
Sigmoidoscopy
Through a sigmoidoscopy, roughly a 15-minute procedure, your doctor will take tissue samples and evaluate your large intestine for any abnormalities in the sigmoid colon (the final part of the large intestine, located just prior to the rectum).
For all people over age 50, sigmoidoscopy is a critical step in checking for colorectal cancer.
Downloadable Forms
Flexible Sigmoidoscopy Form
Small Bowel Endoscopy
This procedure is performed to examine your small intestine and detect any issues.
The first part of your small intestine, as well as your stomach, and esophagus, are primary areas where serious digestive conditions such as gastrointestinal (GI) bleeding, cancer, polyps, and inflammatory bowel disease (IBD) may originate and threaten your health. Due to the location and nature of the small intestine, it can be difficult to view these areas, and thus diagnose these serious medical conditions (where they exist), through other testing methods.
Transoral Incisionless Fundoplication Procedure (TIF)
The transoral incisionless fundoplication procedure, or TIF, is an advanced endoscopic procedure that provides relief from the symptoms of acid reflux associated with chronic gastroesophageal reflux disease (GERD). This minimally invasive procedure treats GERD at its source by repairing the antireflux valve and restoring the body’s natural protection against reflux.
Benefits of this approach include faster recovery time and reduced incidence of long-term side effects when compared with traditional laparoscopic Nissen fundoplication. If necessary, the procedure can be combined with a minimally invasive laparoscopic hiatal hernia repair. The TIF procedure can also be revised if necessary, so your future treatment options are not limited. There are no incisions, no scars, and no metal implants, and the procedure generally takes less than an hour to complete. You may be able to return home the day after your procedure, and return to work and most normal activities within a few days following the procedure.
Upper GI Endoscopy
Your mouth, stomach, and esophagus are all part of your upper GI tract, which performs important functions for your digestive system. To determine whether your upper GI tract is functioning properly, a fiber-optic scoping device will be used during a procedure known as an esophagogastroduodenoscopy (EGD), or upper GI endoscopy.
It’s important to be aware of and maintain health in your upper GI tract, as it can be affected by a number of internal and external factors, including food, infection, and genetics. Conditions that can affect your upper GI tract include:
• Gastritis (inflamed stomach lining)
• Stomach and esophageal tumors
• Indigestion
• Ulcers
• Upper abdominal pain
• Heartburn
• Intestinal bleeding
• Difficulty swallowing
An upper GI endoscopy is vital in effectively detecting and treating these issues.
Downloadable Forms
EGD Instructions Form
Esophagogastroduodenoscopy Information Form